-
Case 1 – Frenectomy

This patient came to our office with a high frenula attachment, which caused soft tissue recession and movement of her front teeth. The frenectomy went smoothly and will prevent future recession and tooth movement. Now she smiles more than ever and feels very confident that her smile will remain comfortable and attractive for life.
-
Case 2 – Allograft
This patient came to our office suffering from gum recession and sensitivity to hot and cold caused by this severe recession. We were able cover the recession with an Alloderm graft and eliminate the patient’s sensitivity to hot and cold. What a difference it has made in the patient’s smile – and life!
-
Case 3 – Allograft

This patient was referred to me by her general dentist for an evaluation of receding gums. I determined that her recession and tooth sensitivity was caused by mechanical trauma, tooth malposition, previous orthodontic treatment, and thin biotype. Multiple teeth had severe recession, and approximately 6 to 8 mm of root structure was exposed. I utilized a donor allograft in order to accomplish root coverage and thicken the gum tissue to decrease the possibility of future recession. The patient healed exceptionally well and without complications. After six weeks, surgical success included 100% root coverage and a thicker gingival tissue that is more resistant to future recession.
-
Case 4 – Soft Tissue Grafting

This patient was referred to me by her dentist for treatment of a gum deformity, recession, and inflammation. I diagnosed the patient with a mucogingival deformity / lack of keratinized gingiva and recession located in the lower right quadrant. Patient reported a dental history of constant inflammation and swelling with pain. The area was treated with a Free Gingival Graft in order to gain an adequate amount of keratinized gingiva and root coverage. Resolution of the gum deformity was noted after six weeks of healing without any continued complications.
-
Case 5 – Allograft
This patient was referred to my office for evaluation of generalized buccal recession in the maxillary quadrants. Hard tissue charting showed approximately 4 to 5 mm of recession on multiple teeth in the upper left and upper right areas. Pre-operative pictures were taken. I recommended a modified tunneling technique utilizing a Perioderm Allograft as the best option for the patient. The procedures were completed in one appointment and patient was released. Post-operative re-evaluation was completed 10 days and 6 weeks. At the 6-week post operative appointment final pictures were taken. The surgical procedure produced 100% root coverage, increase in soft tissue thickness, and complete resolution of the recession.
-
Case 6 – Allograft
This patient was referred to my office for evaluation of generalized buccal recession in the maxillary quadrants. Hard tissue charting showed approximately 4 to 5 mm of recession on multiple teeth in the upper left and upper right areas. Pre-operative pictures were taken. I recommended a modified tunneling technique utilizing a Perioderm Allograft as the best option for the patient. The procedures were completed in one appointment and patient was released. Post-operative re-evaluation was completed 10 days and 6 weeks. At the 6-week post operative appointment final pictures were taken. The surgical procedure produced 100% root coverage, increase in soft tissue thickness, and complete resolution of the recession.
-
Case 7 – Allograft
This patient was referred to me by another Oklahoma City specialist. I determined that his recession and tooth sensitivity was caused by laser induced trauma. A single tooth presented with an irregular contour and localized bone necrosis. I utilized a donor allograft in order to accomplish root coverage and thicken the gum tissue to decrease the possibility of future recession. The patient healed exceptionally well and without complications. After six weeks, surgical success included 100% root coverage and a thicker gingival tissue that is more resistant to future recession.
-
Case 8 – Allograft
In this case, I utilized an allograft donor tissue to accomplish root coverage and increase the gingival tissue. The benefit of using an allograft is the lack of a second surgical site to harvest tissue. I find that patients exhibit less pain and complications when this procedure is performed. After 6 weeks of healing an after picture was taken to compare with how the patient initially presented. Also, the patient reported a decrease in sensitivity to cold liquids and was very pleased with the esthetic outcome.
-
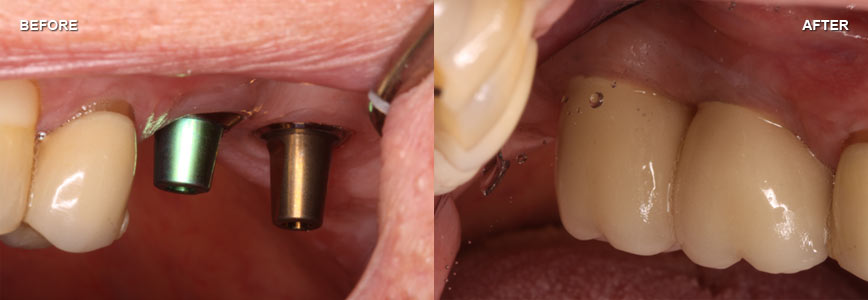
Case 9 – Implants
A patient of record presented with an unrestored #4 (premolar) implant. The dental implant was fully integrated and was ready for restorative treatment. Clinically, I noted that #3 (molar) had an isolated 8 mm probing depth on the palatal root. An x-ray was taken of the area with a gutta percha tip, and a radiolucent area was noted. Surgical examination revealed a vertical root fracture and the tooth was extracted with a bone graft preservation. Approximately 4 months post operatively, a Straumann 4.8mm WN was placed in parallel with #4 implant. The patient was referred to her general dentist for zirconia porcelain implant restorations.
-
Case 10 – Implants
The current patient was referred to me for treatment of two hopeless posterior teeth due to recurrent decay and failing root canal. The hopeless teeth were extracted and grafted with MTF DFDBA cortical particles and a resorb-able membrane. The patient was allowed to heal for approximately six months and no complications were noted. During this time the patient’s body regenerated bone height and width for proper placement of dental implants. Two Straumann wide neck dental implants were placed in proper occlusion. The dental implants osteointegrated over three months of healing. Two solid abutments were torqued into the implants and the patient was referred to his general dentist for permanent crowns. The patient was very satisfied with how dental implants helped replace his hopeless teeth and regain function.
-
Case 11 – Implants
This patient presented with hopeless upper left maxillary teeth due to severe bone loss due to periodontitis. Therefore, extractions of maxillary left posterior teeth was completed with a simultaneous lateral maxillary sinus augmentation. This was done in order to gain vertical alveolar ridge height for proper dental implant placement. After approximately 5 months of healing, 3 Straumann tissue level dental implants were placed with immediate temporization. The patient was referred back to his general dentist for impressions and fabrication of permanent restorations. After occlusal adjustment and proper fit, the restorations were cemented. The cementation of the restorations was concluded approximately 3 months after implant placement.
-
Case 12 – Implants
This case is an example of a patient that was referred to me from her general dentist for a single dental implant. A complete exam was performed for proper diagnosis and rule out any additional problems. Clinically, the Oklahoma City patient presented with a symptomatic abscess on a posterior tooth. Therefore, I extracted the tooth and removed any infectious tissue. A bone graft was utilized to re-establish proper bone height and width. After healing a Straumann dental implant was surgically placed and allowed to integrate with the surrounding regenerated bone. The patient was referred to her dentist for a crown to be fabricated.
-
Case 13 – Implants
The current OKC patient presented with multiple failing teeth due to acute infections. She was only interested in treatment options that were not removable and would allow her to function more naturally. I advised her that dental implants are the only option that would meet her criteria. Therefore, I extracted the hopeless teeth and utilized bone grafting techniques that regenerated sufficient bone height and width. After initial healing, I placed 4 Straumann tissue level implants that integrated into her regenerated bone. The patient was referred back to her dentist for final restorative treatment.